January 2024
Old Dog, New Trick?
Deborah V. Gross, MD, FASAM, DABAM, LFAPA
New Year’s Resolutions seem to be falling out of favor. By Day 5 of 2024, when I started working on this newsletter, I’d already seen numerous emails, articles, and commentaries in which people talked about opting out of the whole “resolution” business toward something more positive. The word itself (resolution) has always struck me as rather grim, conjuring images of gritted teeth and an unpleasant, squinty-eyed staring down the barrel of a new year. At this point in my life, I’m pretty grateful just to be in a new year!
Tanya Sichynsky, in her NYT Cooking newsletter, The Veggie, from January 4, told the story of someone whose plan is to focus on resolutions this year as “silly side quests that just exist to wedge more joy into my life.” For example, she resolved to smile at every child she saw. Great, huh? No squinty-eyed gritting of teeth there!
I’ve made my share of harsh, perfectionistic new year’s resolutions, but this year, my preferred mental image is of open arms, open eyes, and an open, grateful mind and heart. In that spirit, to the amusement of some young people I know, including a couple of grandchildren, I am determined to learn how to connect with people on a social media platform. My goal is to be a voice against stigma and to support people seeking recovery from addiction and other mental or emotional struggles.
Cats led me to X (formerly Twitter), for the pure entertainment of watching the videos (Finn and Mia are favorites). Along the way, I saw people using X to connect around recovery efforts, both seeking and offering support.
I’ve been a writer since at least 4th grade, when I wrote a poem called “The Silver Tree.” I’ve been a physician, psychiatrist, and addictionologist for decades. I recently published what I call a “personal workshop” in a three-book set for disordered eating, designed to be used in multiple settings— formal treatment, mutual help groups (e.g., OA or EDA), and by readers on their own. Everyone deserves access to good, research-based information and advice whether or not they can afford or are ready for formal treatment. Surely, I told myself, if I can do all that, I can figure out this new-fangled way to speak out and support people on their journey! If you are such a person, know that I see you and am absolutely in your corner!
At the moment, all I know how to do on X is “heart” the cats and people who catch my eye, so I’ll likely need your help, too! I’ve treated people in psychotherapy for 40 years, and if I’ve said it once, I’ve said it a zillion times: It’s a process, not a race! If we don’t give up, we make progress. And if we make progress and don’t give up, we are on the journey. Progress, not perfection! That’s as true for an old lady trying to learn to use social media as it is for anyone else on a new path to anywhere!
Lately on X, I’ve seen an image that says, “Stigma Kills.” This is flat, unvarnished truth in a two-word sentence. Why do we humans find it necessary to be so judgy with one another sometimes, particularly over things that can’t be helped? If I’m born a certain way, would that not mean Someone (if you believe in a Someone) made me that way? And even you don’t believe in a Someone, why kick a person who’s already down? Whether by inherited illness like addiction or mood disorder, by psychological injury like PTSD, or by general misfortunes in life, what can possibly be gained by rejecting or attacking suffering people?
When I was a young psychiatrist first in practice, the stigma around even depression (prevalence 24% in women and 13% in men) was so great that people who came to see me lived in fear that someone would see them entering or leaving my office, even though in those days I lived and worked in big cities where the likelihood of any one person running into any other one person on any given day was vanishingly small. To ease their fears, I used very little office signage and assured them that, should we meet in public, I would give no indication that I knew them unless they acknowledged me first. In my office, when they said things like, “My family doesn’t believe in therapy” (or medication or mental illness or addiction or treatment…), I would say, “Well, then I guess it’s a good thing this is science and not religion, eh?”
In recent years, the stigma around some things by some people in some places and some situations seems to have eased a bit, though this remains highly dependent on where you live, what you do, and the family you come from. Patients or former patients in public places now sometimes drag people over to meet me, introduce me as their “shrink,” and joke that “everyone knows you have your hands full since they already know I’m crazy.” Confidentiality being what it is, I learned to just smile and say hi.
I wondered over the years whether the relentless publicity around celebrity mental health struggles and/or trips to “rehab” might ease some of the stigma. Or maybe public mental health information campaigns would help. Or, more recently, perhaps the amazing willingness of people to put their most private info on social media meant that things were loosening up. Unfortunately, the research says otherwise. Instead of making people kinder or more accepting toward self or others, the studies so far indicate that the more time people spend on social media, the more unhappy they are. The jury’s still out, but my guess is that it will turn out like most things human–it depends. Food can bring sustenance and pleasure or turn into a weapon of self-destruction. Medication can save lives and ease suffering or contribute to addiction and death. Perhaps our use of modern communication tools will be similar, though my husband still routinely refers to a certain well-known platform as “farce book….”
I can’t count how many times in psychotherapy I have reminded someone that it is inaccurate to compare our insides (emotions, thoughts, beliefs about ourselves) to other people’s outsides (photos of perfect rooms and cakes and children). If we can remember that, perhaps we can turn things around. Social media “transparency” hasn’t altered the strong, dangerous current of stigma that runs through our culture. Perhaps only we humans can do that. Stigma does kill people. It discourages them from seeking help, and without treatment, many addictions and mental illnesses can be fatal. Stigma also prejudices people against themselves, and it’s no respecter of persons. Most physicians, for example, have resources for treatment, but we also have higher than average rates of addiction, suicide, and some mental illnesses, and lower than average rates of seeking help.
HELP IS AVAILABLE!
Call or text: 988. Chat: 988lifeline.org
January 29th is SAMHSA’s 20th Prevention Day!
Share your story of strength and hope, or read other people’s stories at:
www.SAMHSA.gov.
I am one person with one voice. So are you. Together, we can fight stigma. We can talk openly and give people accurate information to counter the mean-spirited, prejudicial nonsense that is stigma. Changing this dark culture of harshness and shame requires thinking and speaking humanely about things that stigma keeps underground in darkness—mental illness, psychological trauma, addiction, depression, eating disorders, and all the rest. The fight against stigma is a fight against ignorance. It’s a vicious circle. Ignorance wins if stigma rules, and if stigma rules, darkness and danger and ignorance continue. My goal this year—besides proving, at least to myself, that this old dog can learn a new trick—is to shine the light and open some doors, maybe even some minds. Join me, won’t you?
Happy New Year!
Dr. Deborah Gross Discusses Journalist Burnout During SPJ Florida.
Know the Dangers of Sober January
Good Self Care is Not Selfish
Co-Occurring Disorders and Domestic Violence
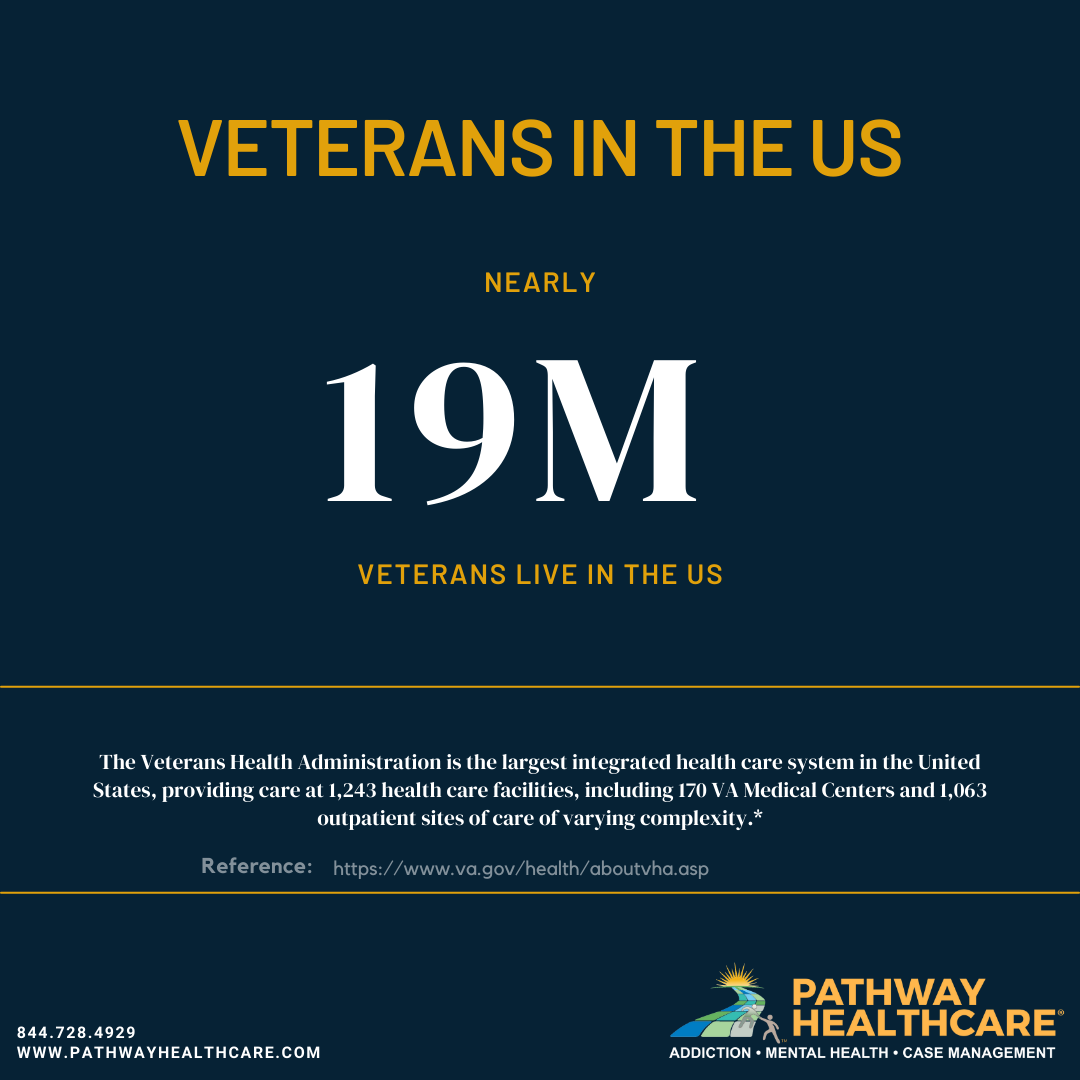
The Five Leading Mental Health Issues Veterans Face and How Pathway Healthcare Can Help
Suicide and Self-Care: Protect Your Risk From One With the Other
Drug overdose deaths increased by more than 20,000 people in 2020
Drug overdose deaths increased by more than 20,000 people in 2020 over 2019, the highest increase on record.
Continue reading